The New Standard of Care in Breast Cancer Screening
Prevention and Treatment Tomosynthesis, an upgraded technology using 3D mammography, is helping Canadians detect breast cancer at an earlier stage. Research is still underway to discover further diagnostic advantages.
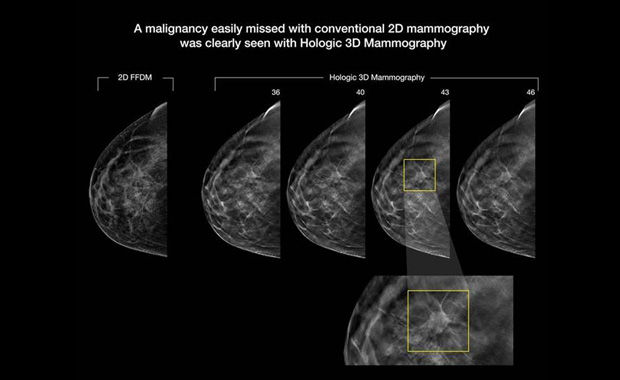
Tomosynthesis, or 3D mammography, is emerging as the new standard of care for breast cancer screening. Traditional digital mammography takes two-dimensional pictures of the breast and remains one of the most advanced tools available for detecting breast abnormalities. However, this x-ray technique does not detect all breast tumors; in fact, up to one-fourth of all cancers may remain undetected, especially in women with dense breast tissue.
“Unlike traditional digital mammography, which takes a two-dimensional x-ray image of the breast, tomosynthesis takes a series of multiple low dose images,” says Dr. Rachel Fleming, Divisional Head of Breast Imaging for the Toronto Joint Department of Medical Imaging (JDMI) in Toronto. “It then combines those images to provide a 3D view so we can actually scroll through the breast and see abnormalities in finer details.”
“It takes away some of the inherent problems with 2D mammography where we have a superimposition of tissues that can mask a cancer or, conversely, appear to be a cancer when in fact they’re not. With 3D mammography we avoid those patients having to come back for further workup,” says Dr. Fleming.
The need for accessible 3D mammography screening
Currently used across Canada as a diagnostic tool after an abnormality is found with 2D mammogram, tomosynthesis is not a widely accessible screening tool. The main reason is reimbursement. There is a higher cost with procuring new tomosynthesis technology, and the test is not covered under some provincial and territorial health insurance plans.
At MIC Medical Imaging in Edmonton, Alberta, where all screening is now done by tomosynthesis (and covered under the province’s health insurance plan), radiologists report positive results. “From the audit of our first full year of using it, we’ve had at least a 50 percent increase in our cancer detection rates,” says Dr. Sheila Appavoo, one of the clinic’s radiologists.
One of those patients was Sue Peters, who credits tomosynthesis for catching her tumour at a very early stage while at the clinic for her screening. “It was only six millimeters at the time of diagnosis — I’m pretty convinced it wouldn’t have been picked up with 2D mammography until it had progressed much further,” says Peters. “It was a much more aggressive cancer, so my treatment plan and outcome could have been completely different had it not been diagnosed for another year or two — I’m very grateful for my extremely early diagnosis and attribute it to the 3D mammography.”
Advocacy is key
Until tomosynthesis becomes universally accesible, women are encouraged to advocate for themselves. “Based on our radiologists’ experience, I encourage my friends and family to get tomosynthesis screening mammography instead of 2D mammography if at all possible,” says Dr. Appavoo, who also encourages fellow radiologists to upgrade to tomosynthesis when their existing mammogram machine becomes obsolete.
